Your Source For The Truth About Locum Tenens:
For Doctors + By Doctors
International locum tenens can be an amazing way to practice medicine abroad—often with strong lifestyle upside and sometimes great pay—but it’s a totally different game than U.S. locums because licensing, visas, and indemnity rules vary by country and can take months to complete. Pick 1–2 target destinations, build a tight credentialing packet, and only accept contracts with crystal-clear scope, pay structure, housing, and malpractice/evacuation coverage so the adventure doesn’t turn into an expensive compliance headache.
Locum tenens travel is basically “ER triage,” but for airports, rental cars, and hotel check-ins—optimize reliability and sleep first, and the money follows. Build a repeatable travel system (direct flights, day-before arrivals, close lodging), and you’ll spend less time getting wrecked by logistics and more time enjoying the freedom locums is supposed to give you.
Locum tenens emergency medicine is the ultimate “choose-your-own-adventure” shift life—more freedom, new EDs, and often better pay, as long as you know what questions to ask and what red flags to avoid. Get your credentials packet tight, pick a safe first site with clear coverage and support, and you’ll turn your first assignment into a smooth, repeatable system (instead of a chaotic travel-and-charting nightmare).
Travel medicine offers doctors a structured, prevention-focused niche centered on pre-travel risk assessment, vaccines, and prophylaxis, while locum tenens provides flexible, temporary assignments that let physicians practice their existing specialty across different locations. This guide explains how each path works—and how to choose or combine them—by breaking down training, workflow, credentialing, malpractice, pay structures, licensing, taxes, and lifestyle considerations.
Locum tenens is temporary physician work where doctors fill short-term staffing needs at hospitals and clinics, offering flexibility, travel opportunities, and often higher hourly pay. This guide explains how locum tenens works from licensing and credentialing to contracts, malpractice, pay, taxes, and how to choose the best locum tenens assignments.
H-1B and J-1 visas affect locum tenens very differently: a J-1 (training) is tightly tied to an approved program and often leads to a waiver pathway with strict, site-specific obligations, while an H-1B is generally more workable for locums but still requires employer/worksite-specific compliance (you can’t freely hop between sites without the right structure). For visa-holding physicians, the safest approach is to pick assignments only after confirming the sponsoring employer, approved worksites, and contract terms (call, cancellations, malpractice, and classification) align with immigration rules—ideally reviewed by an experienced physician-immigration attorney.
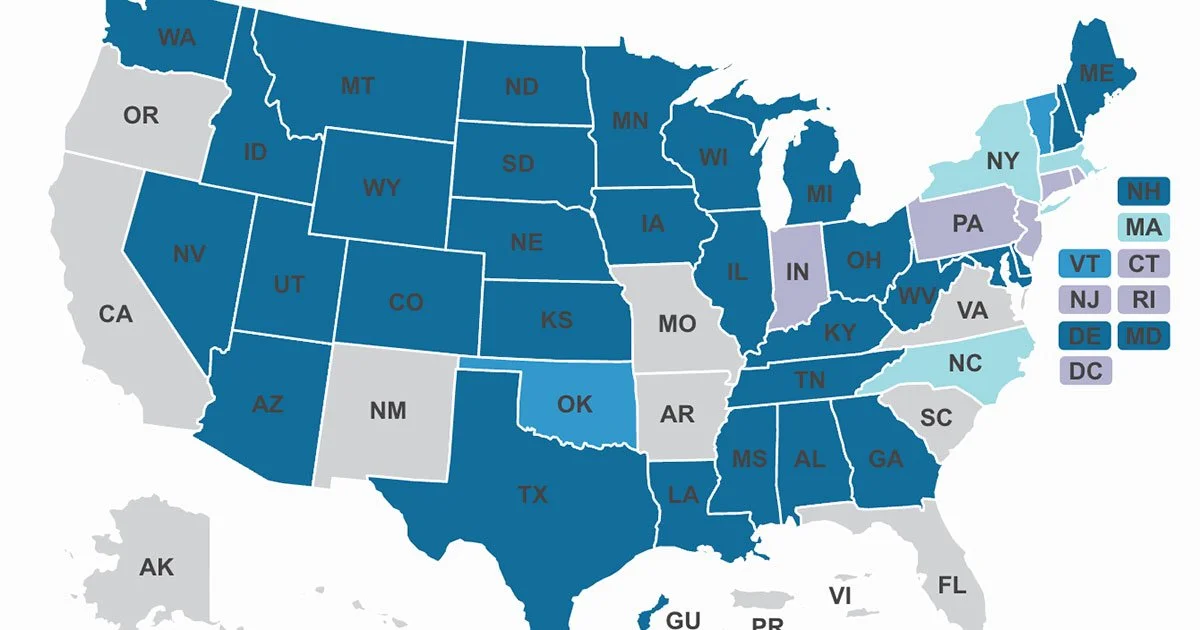
The Interstate Medical Licensure Compact (IMLC/IMLCC) is an expedited pathway that helps physicians doing locum tenens obtain multiple state medical licenses faster, but it does not create one “multi-state license”—each Compact state still issues its own full license, and you must be licensed in the patient’s state (including telehealth). Through the IMLC, you apply via your State of Principal License (SPL) to receive a Letter of Qualification (LOQ)(typically the longest step), then use the Compact process to request expedited licenses in other member states; timelines are often measured in weeks, but background checks, fingerprints, and board processing can still delay starts. Costs include an initial Compact fee plus each state’s license fees and ongoing renewals, so the IMLC is most valuable for locums clinicians who plan to maintain a multi-state footprint (anchor states + opportunity states) and who start the process before they urgently need a new license.
Locum tenens work rewards speed: the faster you can secure and maintain state licenses, the more shifts you can accept—often with better pay and better scheduling leverage. Unfortunately, medical licensure is paperwork-heavy, repetitive, and slow because state medical boards typically require primary-source verification (PSV) of key credentials (medical school, training, identity, exam history, etc.).
If you’re relocating your medical practice or starting multi-state locum tenens, understanding how to transfer a DEA number between states is critical for staying compliant and avoiding credentialing delays. Many clinicians search “DEA transfer,” “move DEA registration to another state,” or even “transfer DEA license,” but the process usually means updating your DEA registration address when you move—or obtaining separate DEA registrations for each statewhere you prescribe controlled substances. In this guide, we break down the exact steps to change your DEA registration when changing states, what to do if you’ll be practicing in multiple states, how state licensing and controlled substance requirements affect your timeline, and the most common mistakes that slow down hospital credentialing.
“Whenever a doctor cannot do good, he must be kept from doing harm” ~Hippocrates












This guide walks doctors through everything they need to know before starting their first locum tenens assignment, with a practical 50-point checklist covering how to choose the right job, lock down scope and contract terms, understand pay/call/guarantees, verify malpractice coverage, complete credentialing and compliance, manage DEA/state requirements, handle travel and housing logistics, and succeed clinically in a new system (EHR access, workflows, escalation pathways, handoffs, documentation, and follow-up responsibilities). It also includes a detailed FAQ that answers the most common first-time locums questions—helping physicians avoid surprises like scope creep, unpaid time, credentialing delays, and unsafe coverage—so the first assignment is predictable, efficient, and burnout-resistant.